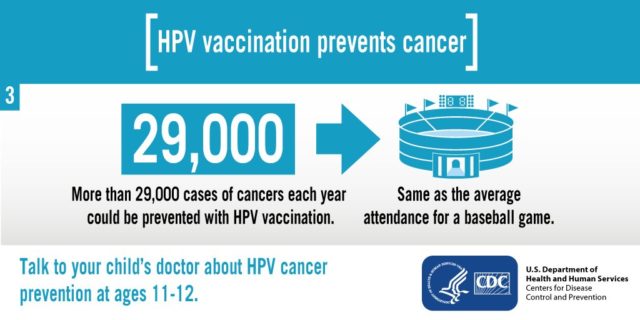
As the days of summer wane and school physicals and forms start to pour into the office, the question never fails. “Do we need any shots?” As many of my patients know, I prefer to call immunizations “protections” and the word “need” can be so loosely interpreted. Many patients use this phrase to refer to what vaccines are needed for school regulations. My hope is that my patients will use this phrase to refer to which vaccines I recommend for them. I get virtually no pushback when I recommend a child or adolescent “needs” protection from meningitis, tetanus, pneumonia, blood stream infections, and a host of other deadly, debilitating, or just plain miserable diseases. However, I often get a lot of questions when I mention a vaccine that prevents cancer, lots of cancer. Human Papilloma Virus (HPV) is estimated to cause 17,600 cases of cancer per year in women and 9,300 cases of cancer in men every year in the United States alone. The vaccines currently available provide near 100% protection against the most common strains of HPV causing these cancers. Even with less than optimal vaccination rates, the CDC has seen a 50% decrease in HPV transmission. With the recent release of Gardasil 9, these numbers should get even better. The nine indicates the number of high risk strains of the virus against which the vaccine provides protection. Previously released vaccines covered two and four strains. So why, with all of this great news, does this vaccine generate so much controversy? For starters, the cancers are often of the mouth, throat, cervix, vulva, anus, and penis and the vast majority are transmitted sexually. While I think most parents are enthusiastic to protect these areas of their child’s body from harm, most seem to be equally uncomfortable thinking about the method in which their child may contract such a virus. As a parent of four children and a pediatrician, I hope both your children and mine make choices in their lives that never put them at risk for HPV. However, that would involve one of two scenarios. One would involve a life of complete abstinence and the other would require that both parties have been completely abstinent previously. While these are certainly admirable and attainable goals, the reality is that not all will achieve them. I hope your child is NEVER exposed to HPV, just like I hope that he or she is never exposed to meningitis, tetanus, or other bad things. But just in case they are, isn’t it nice to know you protected them in some way? The second concern I often hear about the vaccine relates to timing. The vaccines against HPV are recommended at ages 11-12 years. Many parents feel that, even if their child may benefit from this vaccine one day, they certainly do not need it now. I don’t recommend any vaccines because I am just worried about you needing the protection today or tomorrow; I recommend them so that you are protected well before you ever need it. Also, the data has shown the vaccine builds up its strongest antibody response (the thing that makes vaccines work) when given at this age. The last concern I hear relates to safety and the fact that HPV vaccines are relative newcomers. The answer to this is simple: HPV vaccines are currently in their tenth year of recommendation and there is ample data that shows the safety and side effect profile of HPV vaccines to be in line with that of all other standard vaccines. In a time where it feels harder and harder to protect our children from the dangers of the world, HPV vaccination is an opportunity to do just that!